What is a Lipid Profile and Why You Should Know!
Reduce Your Risk Factors for Heart Disease with a Lipid Profile
Intro
Knowing your cholesterol levels is an essential part of understanding your own risk for heart disease. The American Heart Association recommends that everyone over age 20 get a cholesterol test, known as a lipid profile.
Convenient and inexpensive, the lipid profile reveals important information about the types, amount and distribution of the various types of fats (lipids) in your bloodstream. These tests have been shown to be good indicators of whether you are likely to have a heart attack or stroke caused by blockage of blood vessels or hardening of the arteries.
The results of the lipid profile and other known risk factors of heart disease are considered in order to develop treatment and follow-up. Depending on your lipid profile results and other risk factors, treatment options may involve changes to diet and exercise or lipid-lowering medications such as statins.
In the Body Financial, you can think of a lipid profile as a simple, inexpensive type of financial planning. You review the essential numbers for all your related heart health accounts, assess the risk factors, and then take appropriate steps and counter-measures to reduce the risk and create a healthy portfolio.
Why It Matters
Let’s start by putting a very positive perspective on the cholesterol in your body.
Cholesterol is a type of fat, found in your blood. It is produced by your body and also comes from the foods you eat, such as animal products. Cholesterol is needed by your body to maintain the health of your cells. Cholesterol is produced by the liver, circulated by the bloodstream and found in all of the body’s cells. It helps form cell membranes, certain hormones, Vitamin D, tissue, and helps process dietary fats.
There are multiple forms of cholesterol circulating in the blood. The various forms of cholesterol and other fats in the blood are together called lipids. Your blood cholesterol level is related to the foods you eat or to genetic conditions.
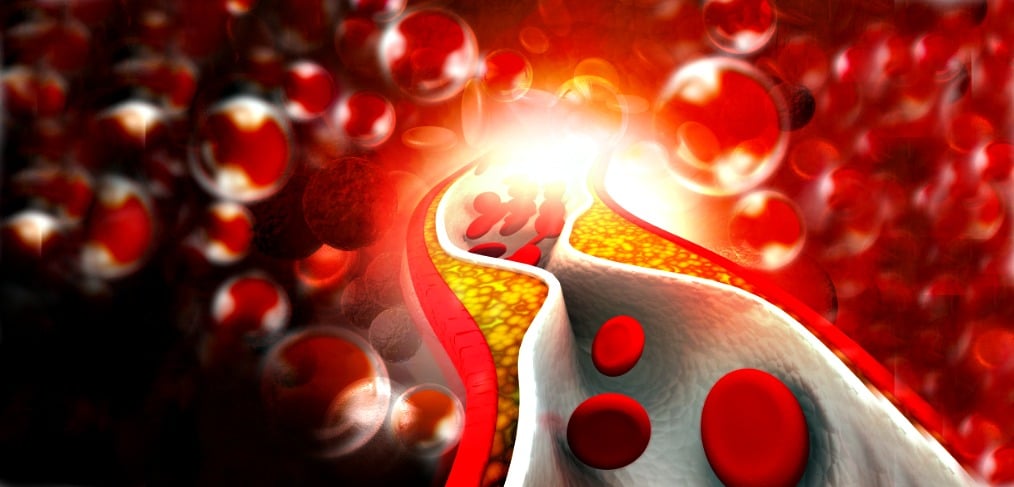
Too much cholesterol is a leading risk factor for heart or coronary artery disease. Cholesterol, together with other substances, can build up inside the walls of the arteries that feed the heart and brain, forming a thick, hard deposit that can clog those arteries. When the blood flow is blocked, or partially blocked, to the heart muscle, the heart starves for oxygen, and a heart attack may result. If a clot blocks blood flow to part of the brain, a stroke may occur.
Lipid Test
Experts recommend follow-up cholesterol testing every five years for most people. People with abnormal lipid panels, or who have other risk factors, may need more frequent cholesterol exams. You can measure high cholesterol with a simple blood test, often called a lipid profile. The lipid profile is usually administered after you have fasted for nine to 12 hours to eliminate the contribution of any fat you recently ate.
Tests for cholesterol provide results for four different types of lipids:
Total Cholesterol
Total Cholesterol is directly linked to risk of heart and blood vessel disease.
LDL, also known as the “bad cholesterol”
LDL is a low-density lipoprotein (combination of fat and protein) found in the blood. It has been called the “bad” cholesterol because it picks up cholesterol from the blood and takes it to the cells. LDL can deposit in blood vessel walls, and over time clog arteries in the process called atherosclerosis. Arteries in the heart narrowed by atherosclerosis can then develop sudden blood clots, causing heart attacks. This is why having high levels of LDL could mean increased risk of heart and blood vessel disease. For your LDL number, lower is better.
HDL, also known as “good cholesterol”
HDL is a high-density lipoprotein, and is called the “good” cholesterol because it removes excess cholesterol from the blood and takes it to the liver. A high HDL level is related to lowering the risk of heart and blood vessel disease. For HDL, the good cholesterol, the more you have of it the better. It protects you and reduces the risk of heart disease.
Triglycerides
Triglycerides are a type of fat found in the blood. The blood level of this type of fat is most affected by the foods you eat, including sugar, fat and alcohol. You can have high triglycerides due to being overweight, having thyroid or liver disease, diabetes and genetic conditions. High levels of triglycerides are related to a higher risk of heart and blood vessel disease.
Lipid profiles can also measure VLDL (very-low-density-lipoprotein) and determine the ratio of good cholesterol to total cholesterol. Having high total cholesterol, high bad cholesterol, or low good cholesterol could place you at higher-than-average risk for heart disease.
The Lipid Lifestyle
Less-than-passing grades on a cholesterol test should be a cause for concern, but those low grades can also be the nudge and extra motivation you need to create a healthier lifestyle. If your lipid panel test results aren’t what you hoped for, it’s time to take action. Identify and begin those lifestyle changes that you can control, the personal effort that helps get your numbers where they need to be.
Remember that multiple factors besides cholesterol contribute to heart disease: diabetes, smoking, high blood pressure, obesity, exercise levels, and genetics. Since many factors contribute to heart disease, abnormal cholesterol does not mean case closed. Far from it. You can have normal cholesterol and have heart disease, or have high cholesterol and have a healthy heart. Overall, more people who have high cholesterol will develop heart disease, compared to those with normal cholesterol tests.
Taking Charge
Here’s the low-down on your diet. Eating foods low in saturated fat (7 percent of total calories or less) and lowering cholesterol (200 mg or less daily) can lower that bad LDL cholesterol. Reduce cholesterol in your diet can reduce bad cholesterol as much as 30 percent.
You don’t need to be a runner or speed skater to benefit from aerobic exercise that lowers bad cholesterol (LDL) and increases good cholesterol (HDL). Walking will do just fine. The American Heart Association recommends that everyone reach a minimum of 30 minutes of some form of cardiovascular exercise five to seven days per week. Other low impact aerobic activity includes swimming, biking, using an elliptical trainer or treadmill.
If diet and exercise don’t lower cholesterol levels to your goal, drug treatment may be needed. A variety of medications or combination treatments can lower cholesterol, including statins, the most effective and commonly used cholesterol drugs.
Experts recommend follow-up cholesterol testing every five years for most people. People with abnormal lipid panels, or who have other risk factors, may need more frequent cholesterol exams. In the Body Financial, knowing about high cholesterol is the first step toward lowering it. You will know what to do to reduce your risk of heart disease. The time and effort you make to improve the results on your next cholesterol test will make a difference.


