Prostate health concerns affect millions of men worldwide, yet many remain unaware of the simple screening tools available to detect potential issues early. The prostate-specific antigen (PSA) test stands as one of the most valuable tools in modern preventive healthcare, offering insights into prostate health that can guide treatment decisions and potentially save lives.
Understanding when and how to use PSA testing empowers men to take control of their health journey. While no single test provides all the answers, PSA screening serves as an important first step in identifying prostate abnormalities before symptoms develop, when treatment options are most effective.
Understanding PSA and Its Role in Prostate Health
Prostate-specific antigen is a protein produced naturally by cells in the prostate gland, serving as a biological marker that can indicate various prostate conditions. When measured through a simple blood test, PSA levels provide valuable information about prostate health, though the results require careful interpretation within the context of individual risk factors and medical history. The relationship between PSA levels and prostate conditions isn’t always straightforward, making professional medical guidance essential for proper evaluation.
PSA testing works by measuring the concentration of this protein in the bloodstream. Under normal circumstances, only small amounts of PSA enter the blood circulation. However, when the prostate experiences inflammation, enlargement, or malignant changes, PSA production can increase significantly, leading to elevated blood levels.
What Elevated PSA Levels May Indicate
Several conditions can cause PSA levels to rise above normal ranges. Prostate cancer represents the most concerning possibility, as cancer cells often produce higher amounts of PSA than healthy prostate tissue. However, elevated PSA doesn’t automatically indicate cancer presence.
Benign prostatic hyperplasia (BPH), a non-cancerous enlargement of the prostate common in older men, frequently causes PSA elevation. Similarly, prostatitis—inflammation or infection of the prostate—can temporarily increase PSA levels. Even routine activities like recent sexual activity, vigorous exercise, or a recent digital rectal examination can influence PSA readings.
Understanding these various causes helps explain why PSA testing requires thoughtful interpretation rather than relying on results in isolation. The test serves as a screening tool that identifies men who may benefit from additional evaluation, not as a definitive diagnostic test for prostate cancer.

Who Should Get PSA Testing?
The decision to begin PSA screening involves weighing potential benefits against possible risks, with recommendations varying based on age, family history, and other risk factors. Current medical guidelines emphasize the importance of informed decision-making between patients and healthcare providers. Different risk profiles call for different screening approaches, making personalized recommendations essential for optimal care.
Average-Risk Men
For men at average risk of prostate cancer, most medical organizations recommend beginning discussions about PSA testing around age 50. This recommendation assumes a life expectancy of at least 10 years, as the benefits of early detection are most significant when sufficient time remains for treatment to impact long-term health outcomes.
Men in this category typically have no family history of prostate cancer and belong to ethnic groups with average prostate cancer risk. The decision to start screening should involve careful consideration of individual preferences, health status, and understanding of both potential benefits and limitations of PSA testing.
High-Risk Populations
Certain groups face elevated prostate cancer risk and may benefit from earlier screening initiation. Men with African ancestry should consider beginning PSA discussions as early as age 40-45, as this population experiences higher incidence rates and more aggressive forms of prostate cancer.
Family history significantly influences prostate cancer risk. Men with fathers, brothers, or multiple family members who developed prostate cancer, particularly at younger ages, may warrant earlier screening consideration. The presence of hereditary cancer syndromes or genetic mutations like BRCA2 also elevates risk levels.
Geographic and lifestyle factors can influence risk as well. Men in certain regions with higher prostate cancer rates or those with specific dietary patterns may benefit from earlier or more frequent screening discussions with their healthcare providers.
Recommended PSA Testing Frequency
The frequency of PSA testing depends largely on initial results and individual risk factors, with most guidelines recommending a risk-stratified approach to follow-up intervals. Rather than universal screening schedules, personalized testing frequencies help optimize the balance between early detection benefits and potential screening-related harms. This approach ensures that men with higher risk receive appropriate monitoring while avoiding over-testing in lower-risk individuals.
Low PSA Levels (Under 1.0 ng/mL)
Men with initial PSA levels below 1.0 ng/mL generally face very low risk of developing clinically significant prostate cancer in the near term. Research suggests these men can safely extend their screening intervals to every 4 years, reducing the frequency of testing while maintaining effective surveillance.
This extended interval approach helps minimize unnecessary testing while ensuring continued monitoring of prostate health. However, men in this category should remain alert to any urinary symptoms or other health changes that might warrant earlier re-evaluation.
Intermediate PSA Levels (1.0-3.0 ng/mL)
PSA levels in the intermediate range require more frequent monitoring, typically every 1-2 years. This range represents a transitional zone where prostate cancer risk increases but remains relatively moderate. Regular monitoring helps detect any upward trends in PSA levels that might indicate developing prostate conditions.
The specific frequency within this range often depends on additional factors such as age, family history, and rate of PSA change over time. Men whose PSA levels remain stable may continue with less frequent testing, while those showing gradual increases might benefit from annual monitoring.
Elevated PSA Levels (Above 3.0 ng/mL)
PSA levels exceeding 3.0 ng/mL generally warrant immediate further evaluation rather than routine rescreening. These levels suggest the need for additional diagnostic procedures, such as digital rectal examination, prostate MRI, or potentially prostate biopsy, depending on the clinical context.
The approach to elevated PSA levels requires individualized assessment considering factors like age, overall health, PSA velocity (rate of change), and patient preferences regarding further testing and potential treatment.
What PSA Levels Can Indicate
PSA level interpretation requires understanding that “normal” ranges vary considerably based on age, ethnicity, and individual factors, making context crucial for proper evaluation. While general reference ranges provide guidance, the trend of PSA changes over time often proves more informative than single measurements. Modern approaches to PSA interpretation emphasize the importance of considering multiple factors rather than relying solely on absolute PSA values.
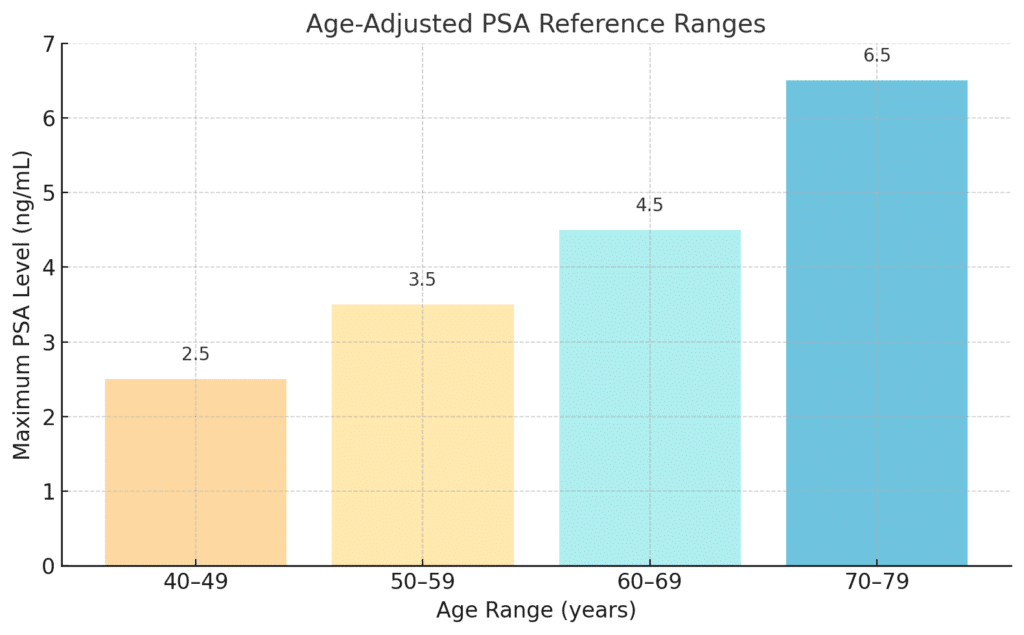
Age-Adjusted PSA Reference Ranges
Prostate size naturally increases with age, leading to corresponding increases in baseline PSA levels. Age-adjusted reference ranges help account for this natural progression:
- Ages 40-49: 0-2.5 ng/mL
- Ages 50-59: 0-3.5 ng/mL
- Ages 60-69: 0-4.5 ng/mL
- Ages 70-79: 0-6.5 ng/mL
These ranges provide general guidance, but individual variation remains significant. Some men naturally produce higher PSA levels without underlying pathology, while others may develop prostate cancer despite PSA levels within typical ranges.
PSA Velocity and Density
PSA velocity measures the rate of PSA change over time, typically calculated as the annual rate of increase. Rapid PSA increases, particularly rises exceeding 0.75 ng/mL per year, may indicate higher likelihood of prostate cancer even when absolute PSA levels remain within normal ranges.
PSA density considers PSA levels relative to prostate size, as determined by imaging studies. This calculation helps distinguish between PSA elevation due to prostate enlargement versus other causes. Higher PSA density values may suggest greater likelihood of cancer presence.
Factors That Can Affect PSA Results
Numerous factors can temporarily or permanently influence PSA levels, making timing and preparation important for accurate results. Recent prostate manipulation, including digital rectal exams, cystoscopy, or prostate biopsy, can elevate PSA levels for several weeks.
Medications also impact PSA readings. 5-alpha reductase inhibitors, commonly prescribed for BPH, can reduce PSA levels by approximately 50%. Testosterone replacement therapy may increase PSA production. Even common activities like bicycle riding, motorcycle riding, or recent ejaculation can temporarily affect results.
Urinary tract infections and prostatitis can significantly elevate PSA levels, sometimes dramatically. These conditions should be treated and resolved before interpreting PSA results for cancer screening purposes.
Next Steps After Elevated PSA
An elevated PSA result initiates a carefully orchestrated evaluation process designed to determine the underlying cause and assess the need for treatment. Rather than immediately proceeding to invasive procedures, modern medical practice emphasizes a stepwise approach that gradually increases diagnostic precision while minimizing unnecessary interventions. This systematic evaluation helps distinguish between various causes of PSA elevation and identifies men who would benefit most from definitive treatment.
Confirmatory Testing and Physical Examination
The first step following an elevated PSA typically involves confirmatory retesting after addressing any factors that might have influenced the initial result. This includes treating any urinary tract infections, avoiding activities that might affect PSA levels, and ensuring adequate time has passed since any prostate manipulation.
A thorough digital rectal examination (DRE) provides valuable complementary information to PSA testing. During this examination, healthcare providers assess prostate size, texture, and the presence of any suspicious nodules or irregularities. The combination of PSA results and physical findings helps guide subsequent evaluation decisions.
Advanced Imaging Studies
Multiparametric MRI of the prostate has revolutionized the evaluation of men with elevated PSA levels. This imaging technique provides detailed visualization of prostate anatomy and can identify suspicious areas that may harbor cancer. MRI results help determine whether prostate biopsy is necessary and can guide the targeting of suspicious regions during biopsy procedures.
The Prostate Imaging Reporting and Data System (PI-RADS) scoring system standardizes MRI interpretation, providing consistent communication between radiologists and urologists. Higher PI-RADS scores indicate greater likelihood of clinically significant prostate cancer and typically prompt recommendations for tissue sampling.
Biomarker Testing and Genetic Analysis
Several advanced biomarker tests can provide additional information about prostate cancer risk in men with elevated PSA levels. These tests analyze various biological markers in blood, urine, or tissue samples to help distinguish between aggressive cancers requiring treatment and indolent cancers that may be safely monitored.
The Prostate Health Index (PHI), 4Kscore test, and SelectMDx represent examples of commercially available biomarker panels that can help refine risk assessment. These tests may help some men avoid unnecessary biopsies or identify those who require more intensive evaluation.
Prostate Biopsy Considerations
When other evaluation methods suggest significant cancer risk, prostate biopsy provides definitive tissue diagnosis. Modern biopsy techniques increasingly utilize MRI guidance to target suspicious areas while sampling representative portions of the entire prostate gland.
The decision to proceed with biopsy involves careful consideration of potential benefits and risks. While biopsy remains the gold standard for prostate cancer diagnosis, the procedure carries risks of infection, bleeding, and temporary urinary difficulties. Shared decision-making between patients and providers helps ensure that biopsy recommendations align with individual values and preferences.

Risks and Considerations of PSA Testing
PSA testing, while valuable, involves several important limitations and potential drawbacks that men should understand before beginning regular screening. The complexity of PSA interpretation and the potential consequences of both false-positive and false-negative results require careful consideration. Understanding these limitations helps men make informed decisions about incorporating PSA testing into their healthcare routine.
False-Positive Results and Overdiagnosis
One of the most significant concerns with PSA screening involves false-positive results—elevated PSA levels in men without prostate cancer. These results can lead to unnecessary anxiety, additional testing, and potentially harmful procedures. Studies suggest that approximately 70-80% of men with elevated PSA levels do not have prostate cancer, highlighting the frequency of false-positive results.
Overdiagnosis represents another important consideration, referring to the detection of slow-growing cancers that may never cause symptoms or affect life expectancy. Many prostate cancers grow so slowly that men die from other causes before the cancer becomes clinically significant. Treatment of these indolent cancers may cause more harm than benefit, leading to unnecessary side effects without improving survival outcomes.
Psychological Impact and Quality of Life
The emotional impact of abnormal PSA results extends beyond medical considerations. Many men experience significant anxiety while awaiting further test results or during the evaluation process. This psychological burden can affect relationships, work performance, and overall quality of life, even when subsequent testing reveals no cancer.
The uncertainty inherent in PSA testing can create ongoing stress for some men. Regular screening may serve as a constant reminder of cancer risk, potentially affecting mental health and well-being. These psychological factors represent important considerations in the decision to begin or continue PSA screening.
Shared Decision-Making Approach
Current medical guidelines emphasize the importance of shared decision-making between patients and healthcare providers regarding PSA screening. Rather than universal screening recommendations, this approach recognizes that the benefits and risks of testing vary among individuals based on their values, preferences, and clinical circumstances.
Effective shared decision-making involves discussing the potential benefits of early cancer detection, the limitations of PSA testing, the possibility of false results, and the potential consequences of both action and inaction. This process helps ensure that screening decisions align with individual goals and priorities.
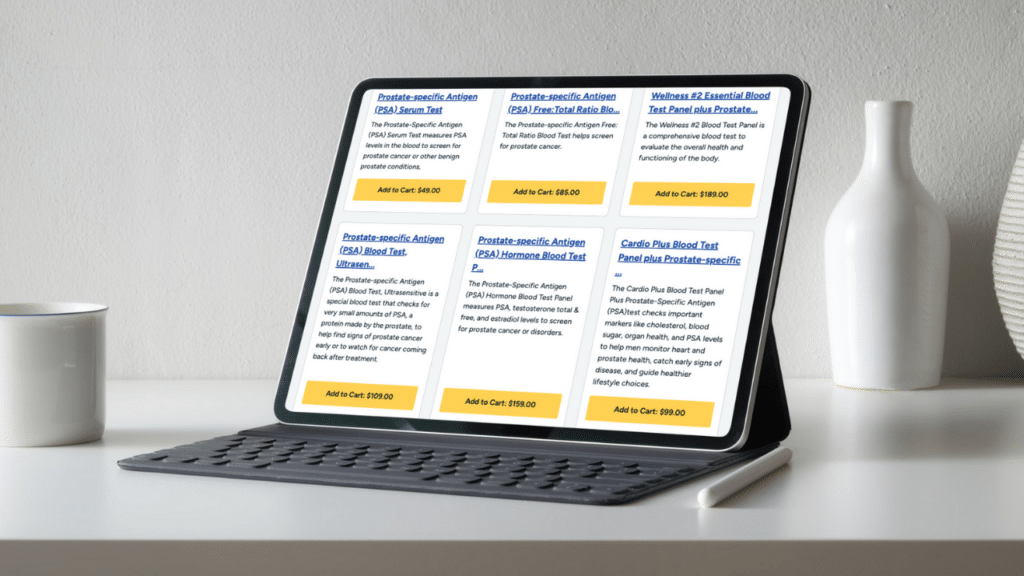
Walk-In Lab Advantage
Access to PSA testing has been simplified through direct-to-consumer laboratory services, offering men convenient and confidential screening options without the traditional barriers of healthcare access. Walk-In Lab provides an efficient pathway for men who want to take proactive control of their prostate health monitoring. This accessibility removes common obstacles that might otherwise prevent men from obtaining important health screenings.
Convenience and Accessibility
Walk-In Lab eliminates the need for doctor’s appointments solely to order PSA testing, allowing men to initiate screening based on their own health awareness and risk assessment. This direct access proves particularly valuable for men with busy schedules, limited healthcare access, or those who prefer to handle routine health monitoring independently.
The nationwide network of laboratory locations ensures that PSA testing remains accessible regardless of geographic location. Extended hours and walk-in availability accommodate various work schedules and personal preferences, making it easier for men to prioritize their health screening needs.
Cost-Effective Testing Solutions
Transparent, upfront pricing eliminates the uncertainty often associated with medical testing costs. Walk-In Lab’s affordable pricing structure makes PSA testing accessible to men regardless of insurance coverage or financial circumstances. This cost transparency allows men to budget for regular screening as part of their preventive healthcare routine.
The elimination of additional fees, facility charges, and administrative costs associated with traditional medical office visits can result in significant savings while maintaining the same laboratory quality and accuracy standards used in conventional healthcare settings.
Confidential Results and Professional Follow-Up
PSA test results are delivered securely and confidentially, allowing men to review their results privately before deciding on next steps. The availability of detailed result explanations helps men understand their PSA levels and determine whether additional medical consultation is warranted.
Walk-In Lab provides results that can be easily shared with healthcare providers for professional interpretation and follow-up care planning. This seamless integration between direct-access testing and traditional medical care ensures continuity and appropriate medical oversight when needed.
Frequently Asked Questions
At what age should PSA testing start?
Men at average risk should begin discussing PSA testing with their healthcare providers around age 50, assuming a life expectancy of at least 10 years. High-risk men, including those with African ancestry or strong family histories of prostate cancer, may benefit from beginning these discussions as early as age 40-45. The decision should always involve careful consideration of individual risk factors, health status, and personal preferences.
What is considered a normal PSA level?
PSA levels naturally increase with age, making age-adjusted reference ranges more meaningful than universal cutoffs. Generally, levels below 4.0 ng/mL are considered normal, but this varies by age. Younger men typically have lower baseline PSA levels, while older men may have higher levels without indicating cancer. The trend of PSA changes over time often provides more valuable information than single measurements.
What factors can affect PSA test results?
Multiple factors can temporarily or permanently influence PSA levels. Recent sexual activity, vigorous exercise, bicycle riding, or prostate manipulation through medical examinations can elevate results. Urinary tract infections and prostatitis significantly increase PSA levels. Certain medications, including 5-alpha reductase inhibitors and testosterone replacement therapy, also affect PSA production. Proper preparation and timing help ensure accurate results.
Does a high PSA level mean I definitely have cancer?
Elevated PSA levels do not automatically indicate prostate cancer presence. Many conditions can cause PSA elevation, including benign prostatic hyperplasia (BPH), prostatitis, and urinary tract infections. Studies show that approximately 70-80% of men with elevated PSA levels do not have prostate cancer, emphasizing the need for additional evaluation to determine the underlying cause.
How accurate is PSA testing for detecting prostate cancer?
PSA testing serves as an effective screening tool but has limitations in diagnostic accuracy. The test can miss some prostate cancers (false negatives) while indicating possible cancer in men who don’t have the disease (false positives). PSA testing works best when combined with other evaluation methods, including physical examination, medical history, and potentially advanced imaging or biomarker testing.
What happens if my PSA level is elevated?
Elevated PSA results typically trigger a systematic evaluation process beginning with confirmatory retesting and physical examination. Depending on the degree of elevation and other factors, additional steps may include prostate MRI, advanced biomarker testing, or prostate biopsy. The specific evaluation pathway depends on individual circumstances, risk factors, and patient preferences discussed with healthcare providers.
How often should I get PSA testing?
Testing frequency depends on initial PSA results and individual risk factors. Men with PSA levels below 1.0 ng/mL may retest every 4 years, while those with levels between 1.0-3.0 ng/mL typically test every 1-2 years. PSA levels above 3.0 ng/mL generally require immediate further evaluation rather than routine rescreening. Personal risk factors may modify these general recommendations.
Can I stop PSA testing at a certain age?
The decision to discontinue PSA testing depends on life expectancy, overall health, and personal preferences. Men with life expectancies less than 10 years may not benefit from continued screening, as the potential harms may outweigh benefits. However, some men choose to continue testing for peace of mind, while others prefer to focus on other aspects of health maintenance.

Conclusion
PSA testing represents a valuable tool in the comprehensive approach to men’s health, offering insights into prostate health that can guide important medical decisions and potentially save lives through early detection. While not perfect, PSA screening provides men with actionable information about their prostate health when interpreted properly within the context of individual risk factors and medical history.
The key to effective PSA testing lies in understanding both its capabilities and limitations. When used as part of a broader health monitoring strategy, PSA testing helps identify men who may benefit from additional evaluation while avoiding unnecessary interventions in those at low risk. This balanced approach maximizes the benefits of screening while minimizing potential harms.
Modern healthcare increasingly emphasizes patient empowerment and shared decision-making, and PSA testing exemplifies this trend. By understanding the role of PSA in prostate health monitoring, men can make informed decisions about incorporating this test into their preventive healthcare routine. Whether obtained through traditional medical visits or convenient direct-access services like Walk-In Lab, PSA testing provides men with valuable information to guide their health journey.
The accessibility and affordability of PSA testing through Walk-In Lab removes traditional barriers to prostate health monitoring, enabling men to take proactive control of their health screening needs. This direct access to quality laboratory testing, combined with professional medical consultation when indicated, represents an optimal approach to modern preventive healthcare.
Ultimately, PSA testing serves as one component of comprehensive men’s health care, working best when combined with regular medical check-ups, healthy lifestyle choices, and open communication with healthcare providers. By understanding what PSA testing can and cannot tell us about prostate health, men can utilize this valuable screening tool effectively as part of their long-term health strategy.
Ready to take control of your prostate health? Order your PSA test today and gain valuable insights into your health status with convenient, confidential, and affordable testing.
Disclaimer: This content is for informational purposes only and should not be used as a substitute for professional medical advice. Always consult with qualified healthcare providers regarding medical conditions, testing decisions, and treatment options.
