Introduction to Gout
Gout is not just a mere inconvenience but a significant inflammatory arthritis with a distinct presentation and progression. The following phrase can be rephrased as: “Frequently misconstrued as a mere dietary mistake, it is actually a medical ailment that can significantly affect a person’s way of life and ability to move.” Excessive uric acid in the bloodstream leads to the formation of sharp urate crystals in a joint or surrounding tissue, resulting in severe pain and inflammation, which are the hallmarks of this type of arthritis.
The condition predominantly affects joints and is most notorious for targeting the metatarsophalangeal joint at the base of the big toe. However, it is not limited to the feet; gout can affect any joint, including knees, elbows, wrists, and fingers. The beginning of a gout episode generally occurs abruptly, resulting in intense pain, swelling, redness, and tenderness in the affected areas, often causing individuals to wake up in the middle of the night.
While gout can appear as isolated incidents known as flares, its recurrent nature can lead to chronic degradation of joint health if not properly managed. These flares are not only extremely painful but also contribute to a cycle of inflammation and damage that may complicate over time, underscoring the importance of understanding and treating gout as more than just a temporary ailment.
Causes and Risk Factors of Gout
The onset of gout is mainly caused by the buildup of uric acid in the blood, which is a result of the body’s metabolism of purines. The usual process involves the kidneys processing uric acid and then excreting it through urine. When the body creates an excessive amount of uric acid or when the kidneys eliminate too little of it, the uric acid can form crystals and accumulate in the joints. This can lead to the typical inflammatory reactions associated with gout.
The development of this condition can be impacted by a range of genetic, dietary, and physiological elements. Genetic composition is particularly influential, as people with a family history of gout have a higher likelihood of experiencing the condition themselves. This predisposition combined with other health conditions, such as metabolic syndrome, obesity, and chronic kidney disease, can further exacerbate the risk.
Lifestyle choices heavily impact uric acid levels. Diets rich in purines—substances found in high concentrations in certain meats, seafood, and alcoholic beverages—can increase the production of uric acid. Consumption of sugary beverages is also linked to higher uric acid levels. On the other hand, dietary adjustments, such as reducing intake of high-purine foods and alcohol, can significantly help manage gout symptoms and prevent flare-ups.
It’s important for those at risk of gout to understand these factors, as recognizing and modifying them can lead to effective management and prevention of gout episodes. Individuals can minimize the effect of this condition on their everyday lives by making appropriate lifestyle adjustments and acquiring the necessary knowledge.

Symptoms and Progression of Gout
Gout’s hallmark is its acute attacks, which can strike suddenly and are often excruciatingly painful. Episodes of this nature often present as severe discomfort in the joints, predominantly in the large toe, but may also affect other areas such as the knees, elbows, wrists, and fingers. The impacted joint swells, becomes red, and feels warm, significantly restricting movement and causing substantial discomfort. These symptoms often begin at night, escalating rapidly to peak intensity within 12-24 hours of onset.
Stages of Gout:
Gout progresses through several stages, starting with asymptomatic hyperuricemia, where high uric acid levels are present in the blood but without any outward symptoms. This stage can last for years without the individual realizing they have a condition that could potentially lead to gout.
The next phase is acute gouty arthritis, where urate crystals trigger sudden inflammation and pain in the joints. These flares can last from a few days to several weeks, often followed by periods known as inter-critical periods. During these intervals, the individual typically experiences no symptoms, and the condition may seem to have resolved; however, without treatment, gout can progress to more frequent and severe attacks.
The final and most debilitating stage is chronic tophaceous gout. In this advanced phase, the continuous accumulation of urate crystals leads to the formation of tophi—hard, uric acid deposits that can cause joint deformity and chronic pain. At this stage, the inflammation may become persistent, leading to joint damage and a decrease in quality of life.
Understanding the symptoms and stages of gout is essential for timely diagnosis and effective management. With appropriate treatment, the progression of gout can be significantly slowed or even halted, preventing the condition from reaching the severe stages that cause irreversible damage.
Diagnosis and Monitoring of Gout
Diagnosing gout involves several key steps that help distinguish it from other types of arthritis. Blood tests are commonly used to measure uric acid levels, which are typically elevated in gout patients. However, high uric acid alone does not confirm gout, as levels can fluctuate, especially during an attack. For a definitive diagnosis, joint fluid analysis is conducted. This procedure involves extracting the fluid from the joint that is affected and examining it under a microscope for urate crystals—the telltale sign of gout.
Once diagnosed, the management of gout doesn’t end with treatment of acute attacks. Regular monitoring is essential to effectively control the condition and prevent its progression. Periodic blood tests are recommended to measure uric acid levels as they provide a gauge of how well the current treatment is working. Monitoring helps in adjusting medications to achieve optimal uric acid levels and prevent the formation of new urate crystals.
Moreover, regular check-ups provide an opportunity to assess the need for changes in medication dosages or lifestyle adjustments. These evaluations are crucial because they help prevent the recurrence of gout attacks and reduce the risk of complications, such as the development of tophi or chronic joint damage.
Understanding the critical roles of diagnosis and monitoring can empower patients to take an active part in managing their gout, ensuring better outcomes and a higher quality of life.
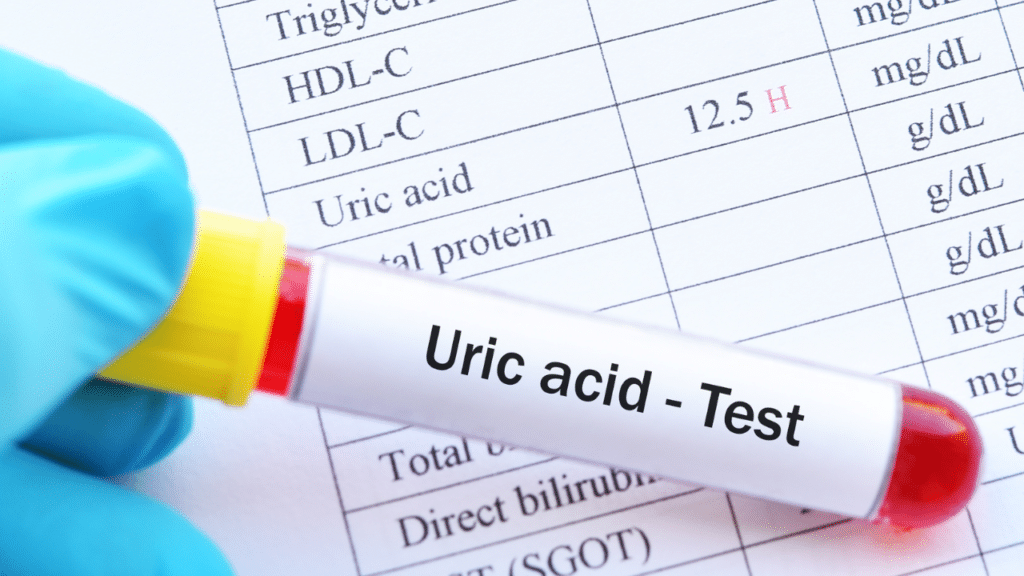
A blood test for uric acid can be useful in diagnosing gout. Elevated uric acid levels in the bloodstream are associated with the development of gout. For the majority of individuals, normal uric acid levels range from 3.5 to 7.2 milligrams per deciliter (mg/dl).
Source: https://www.kidneyfund.org/
Treatment Options for Gout
Managing Acute Attacks
The primary goal in treating acute gout attacks is to quickly alleviate pain and inflammation. Non-steroidal anti-inflammatory drugs (NSAIDs) are often the first line of treatment, providing significant relief from the intense pain associated with gout flares. For those who cannot take NSAIDs, corticosteroids or colchicine may be prescribed. These medications are most effective when taken at the first sign of an attack, highlighting the importance of early intervention.
Long-term Management
In addition to treating acute episodes, long-term management focuses on reducing and maintaining lower uric acid levels to prevent future attacks and potential joint damage. Urate-lowering therapies are central to this strategy. Allopurinol and febuxostat commonly are used to decrease the body’s production of uric acid. For individuals who continue to experience gout flares despite these medications, or for those who suffer from chronic gout, newer therapies like pegloticase, which helps the body to break down uric acid, can be considered.
Having regular follow-ups with a healthcare provider are essential to monitor the effectiveness of the treatment regimen and make adjustments as needed. This proactive approach helps to manage the disease effectively over the long term and minimizes the risk of complications.
Role of Lifestyle Changes
Making important lifestyle modifications plays a crucial role in managing gout. Making the right dietary changes, such as reducing the intake of high-purine foods (like red meat and certain seafood), avoiding sugary beverages, and moderating alcohol consumption, are vital. Maintaining a healthy weight and engaging in regular exercise also contribute to lowering uric acid levels and reducing the frequency of gout attacks.
Adopting these lifestyle habits can significantly enhance the effectiveness of medications and help to control gout more effectively, leading to a better quality of life for those affected by this condition.

Preventive Measures and Lifestyle Modifications for Gout
Dietary Recommendations
One of the most effective ways to prevent gout attacks and manage uric acid levels is through dietary modifications. Avoiding high-purine foods is crucial; these include red meats, certain seafoods such as anchovies, herring, and mackerel, and organ meats like liver. Instead, incorporating more low-purine foods can make a significant difference. Eating fresh fruits, vegetables, whole grains, and low-fat dairy products not only reduce uric acid levels but also support overall health.
Increasing water intake is another simple yet effective strategy. Adequate hydration can help dilute the uric acid in the bloodstream and facilitate its excretion through urine. Aim for at least eight glasses of water per day, especially if you are prone to gout flares.
Lifestyle Choices
Alongside dietary changes, maintaining a healthy weight is essential in preventing gout. Obesity can increase the body’s production of uric acid and decrease its elimination. Regular exercise, coupled with a balanced diet, can help achieve and maintain a healthy weight, thus reducing the risk of gout.
Moderating alcohol intake is also important, as alcohol can increase uric acid production and reduce its excretion. Beer and spirits, in particular, are high in purines, so reducing their consumption is advisable. Instead, opt for moderate wine consumption or alcohol-free alternatives.
Other beneficial lifestyle modifications include managing stress levels and ensuring adequate sleep, as stress can exacerbate gout symptoms. Regular relaxation techniques and a consistent sleep schedule can help in managing these factors.
By adopting these preventive measures and lifestyle changes, individuals can significantly reduce the frequency of gout attacks and improve their quality of life, managing the condition more effectively and preventing its progression.

Complications and Associated Conditions of Gout
Gout, if left untreated, can lead to a variety of severe complications that not only affect the joints but also other aspects of health. Chronic gout can cause the formation of tophi, which are deposits of urate crystals that accumulate in soft tissues. These deposits can lead to permanent joint damage, resulting in chronic pain and significantly reduced mobility.
Furthermore, the excess of uric acid responsible for gout is also a common culprit in the formation of kidney stones. These stones can cause extreme pain and may lead to more severe kidney problems, including chronic kidney disease, if recurrent.
Beyond the joints and kidneys, gout is also associated with several metabolic and cardiovascular conditions. Research shows a clear link between gout and higher risks of hypertension and cardiovascular diseases. The inflammation and high uric acid levels seen in gout may also exacerbate conditions like diabetes and metabolic syndrome, complicating the management of these diseases.
Understanding these potential complications emphasizes the importance of managing uric acid levels and treating gout symptoms proactively to prevent more serious health issues. Effective management not only addresses the symptoms of gout but also mitigates the risks of associated conditions, providing a holistic approach to health that extends beyond the joints.
Gout is a type of arthritis. Specifically, it is an inflammatory arthritis caused by the deposition of urate crystals in the joints, which leads to sudden and severe episodes of pain and swelling. These attacks can affect any joint but most commonly occur in the big toe. Gout develops due to high levels of uric acid in the blood, which can form sharp, needle-like crystals in a joint or surrounding tissue, causing intense pain, inflammation, and redness.

Take Action!
In conclusion, gout is a serious form of arthritis that, if left unchecked, can lead to debilitating pain and irreversible damage to the joints. Recognizing that gout stems from the build-up of urate crystals, it becomes crucial to understand both its acute manifestations and its chronic implications. Effective management of gout involves a combination of medical treatment to control symptoms and prevent future attacks, as well as lifestyle modifications that can significantly reduce the risk of flares and associated health complications.
Early diagnosis and ongoing management are essential for maintaining quality of life and avoiding severe outcomes such as joint destruction and kidney disease. The link between gout and other significant health conditions such as cardiovascular disease and diabetes emphasizes the need for a holistic health strategy, especially for individuals at greater risk.
If you suspect you might be suffering from gout or if you have a family history of this condition, don’t hesitate to get medical advice and order a Uric Acid Test at Walk-In Lab. Effectively managing gout requires a partnership between you and your healthcare provider to tailor a treatment and prevention strategy that fits your unique needs.
We also encourage you to share your experiences or ask questions in the comments below. Engaging with others who face similar challenges can provide not only support but also new insights into managing this painful condition.