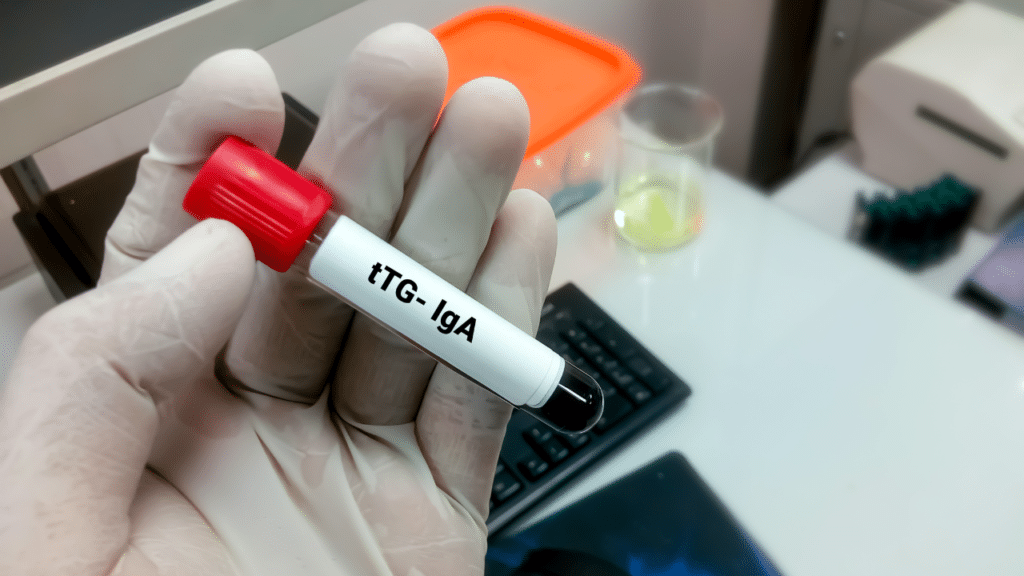
The Tissue Transglutaminase (tTG) Blood Test is one of the primary tools used to diagnose celiac disease. The tTG test measures the level of antibodies that are produced by the immune system in response to the enzyme tissue transglutaminase, which is found in the small intestine. Specifically, it detects Immunoglobulin A (IgA) antibodies, which are typically elevated in individuals with untreated celiac disease.
The tTG blood test is valued for its accuracy and reliability. It possesses a high level of sensitivity and specificity, allowing it to accurately distinguish individuals with celiac disease from those without the condition. The procedure for taking the tTG blood test is straightforward. A healthcare provider draws a blood sample, which is then analyzed in a laboratory for the presence of tTG IgA antibodies.
For the test to be most accurate, it’s essential that the individual continues to consume gluten before and during the testing period. Not eating food with gluten can lead to a decrease in antibody levels, potentially resulting in a false-negative result. Therefore, patients are typically advised to maintain their regular diet until all testing is complete.
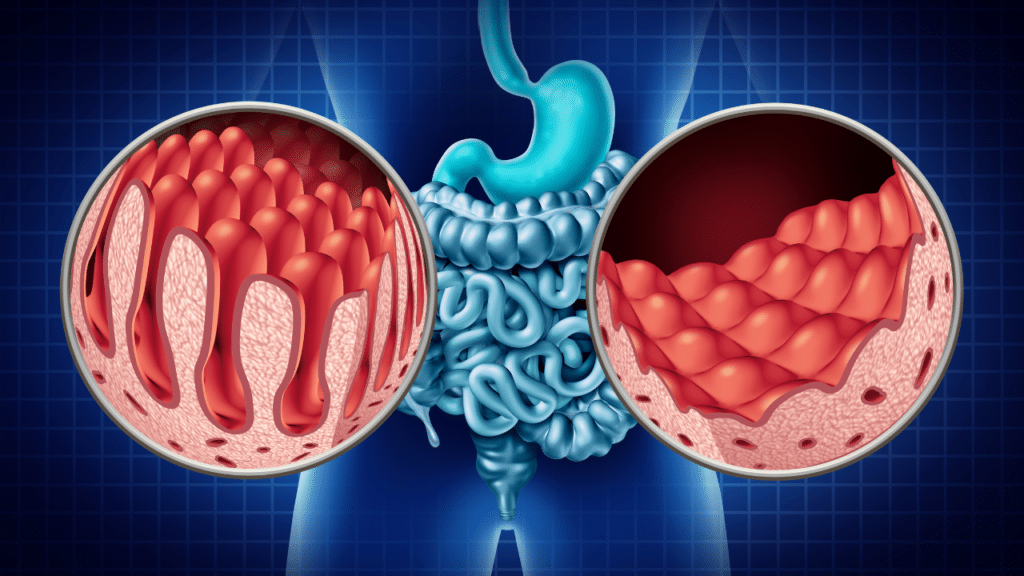
The presence of tTG IgA antibodies in the blood suggests that the body’s immune system is reacting to gluten by attacking the tissue transglutaminase enzyme. This immune reaction is a hallmark of celiac disease and helps to distinguish it from other gluten-related disorders. However, while a positive tTG blood test strongly indicates celiac disease, it is usually confirmed with an intestinal biopsy to assess the extent of damage to the villi in the small intestine.
What the Blood Test Results Show
The results of the Tissue Transglutaminase (tTG) Blood Test can provide crucial information about whether someone has celiac disease. Here’s what different outcomes might indicate:
Positive Test Result
A positive tTG IgA blood test result means that the immune system has produced antibodies against tissue transglutaminase, suggesting an immune response to gluten. This strongly indicates the presence of celiac disease. However, a positive result is typically followed by an intestinal biopsy to confirm the diagnosis. During the biopsy, a small tissue sample from the small intestine is examined for damage to the villi, which is characteristic of celiac disease.
Negative Test Result
A negative tTG IgA blood test result generally means that celiac disease is unlikely, particularly if the individual has been consuming gluten regularly. However, it’s important to consider other factors that might influence the result. For example, some people with celiac disease might have selective IgA deficiency, which means they produce little or no IgA antibodies. In such cases, an alternative test measuring IgG antibodies might be necessary.
False Positives and False Negatives
While the tTG blood test is highly sensitive and specific, false positives and negatives can occur. A false positive might happen due to other autoimmune conditions, like type 1 diabetes or autoimmune liver disease, which can also produce tTG antibodies. Conversely, a false negative could result if the person has been on a gluten-free diet before the test or has selective IgA deficiency.
Sensitivity and Specificity
The sensitivity of the tTG blood test, which refers to its ability to correctly identify those with celiac disease, is around 98%. Its specificity, which measures its ability to correctly identify those without the disease, is also about 98%. These high percentages make the tTG test a reliable initial screening tool.
Given these possibilities, it’s essential to interpret the tTG blood test results in the context of a complete clinical evaluation. Physicians often consider symptoms, family history, and the results of additional tests to make a comprehensive diagnosis. A positive tTG test followed by a confirming biopsy provides a definitive diagnosis of celiac disease, enabling patients to begin a treatment plan that includes a strict gluten-free diet.

Additional Blood Tests for Celiac Disease
While the Tissue Transglutaminase (tTG) Blood Test is the primary test for diagnosing celiac disease, other blood tests can provide additional information and help confirm the diagnosis. Here are a few commonly used tests:
Total Serum IgA
The total serum IgA test measures the overall level of Immunoglobulin A (IgA) in the blood. This test is important because a deficiency in IgA can lead to false-negative results in the tTG IgA test. If an IgA deficiency is detected, doctors may use other types of antibody tests that do not rely on IgA.
Deamidated Gliadin Peptide (DGP) Antibodies
The DGP antibody test measures the immune response to deamidated gliadin peptides, which are modified fragments of gluten. This test can detect both IgA and IgG antibodies against DGP. It is particularly useful in individuals who have an IgA deficiency or in young children where the tTG test might be less accurate.
Endomysial Antibodies (EMA)
The EMA test detects antibodies directed against the endomysium, a connective tissue found in the muscles. Like the tTG test, it is highly specific for celiac disease. However, it is less commonly used because it is more labor-intensive and expensive to perform. When performed, it is often used to confirm a positive tTG result.
HLA-DQ2 and HLA-DQ8 Genetic Testing
Genetic testing for the HLA-DQ2 and HLA-DQ8 genes can help determine the likelihood of developing celiac disease. Most people with celiac disease carry one or both of these genes. However, having these genes alone is not enough to diagnose the disease, as they are also present in up to 30% of the general population. This test is more useful for ruling out celiac disease, as the absence of these genes makes the diagnosis highly unlikely.
These other tests can provide a more comprehensive picture when diagnosing celiac disease, especially in cases where the tTG test results are ambiguous or when an IgA deficiency is present. By combining these tests, healthcare providers can make a more accurate diagnosis and ensure appropriate treatment is started promptly.

What to Do After a Positive Diagnosis
Receiving a positive diagnosis for celiac disease can be overwhelming, but there are clear steps you can take to manage the condition effectively.
Consult with a Gastroenterologist
The first step after a positive tTG blood test is to consult with a gastroenterologist. This specialist will likely recommend an intestinal biopsy to confirm the diagnosis. During this procedure, a small sample of the small intestine’s lining is taken and examined to see if there is damage to the villi, which is a definitive sign of celiac disease.
Transition to a Gluten-Free Diet
Once celiac disease is confirmed, the primary treatment is a strict gluten-free diet. This means staying away from all foods that contain wheat, barley, and rye. Transitioning to a gluten-free diet can be very challenging at first, but it is essential for managing symptoms and preventing further intestinal damage. Many gluten-free alternatives are available, and learning to read labels and identify hidden sources of gluten is crucial.
Consult with a Dietitian
Working with a dietitian or nutritionist who specializes in celiac disease can be incredibly helpful. A dietitian can provide guidance on creating a balanced, nutritious gluten-free diet, help identify hidden sources of gluten, and suggest suitable food substitutes. They can assist with meal planning and provide tips for eating out safely.
Educate Yourself and Your Family
Educating yourself about celiac disease and its management is key. This includes understanding what foods and products to avoid, how to prevent cross-contamination in the kitchen, and recognizing symptoms of accidental gluten ingestion. It is also important to educate family members and friends to ensure they understand the dietary restrictions and can provide support.
Regular Monitoring and Follow-Ups
Having regular follow-ups with your healthcare provider are necessary in order to monitor your condition and ensure you are adhering to a gluten-free diet. Your doctor may periodically repeat the tTG blood test to check for a decrease in antibody levels, indicating that your body is healing and that the diet is effective. Regular bone density tests and assessments for nutrient deficiencies might also be recommended.
Managing Symptoms and Complications
Even with a strict gluten-free diet, some individuals may continue to experience symptoms or develop complications. If symptoms persist, it is important to consult with your healthcare provider to investigate other potential causes and adjust your treatment plan as needed. Nutritional supplements may be necessary to address deficiencies caused by malabsorption, and additional medications might be required to manage specific symptoms or related conditions.
Seek Support
Living with celiac disease can be isolating, but seeking support from people who understand the condition can make a significant difference. Joining a celiac disease support group, either in person or online, can provide a sense of community and a wealth of practical advice. Sharing your personal experiences, tips, and recipes with others who face similar challenges can help you navigate your new lifestyle more easily.
By following these steps and maintaining a gluten-free lifestyle, people with celiac disease can manage their condition effectively, reduce symptoms, and lead a healthy, active life.
Managing Celiac Disease
Effective management of celiac disease goes beyond just adhering to a gluten-free diet. It involves continuous monitoring, nutritional management, and seeking support to ensure overall well-being.
Regular Medical Follow-Ups
Regular follow-ups with a healthcare provider, typically a gastroenterologist, are essential for managing celiac disease. These appointments help monitor the effectiveness of the gluten-free diet and detect any potential complications early. Your doctor may perform periodic blood tests to check for a decrease in tTG antibodies, indicating that the gluten-free diet is working and intestinal healing is occurring. Additionally, bone density tests might be conducted to assess for osteoporosis, a common complication due to nutrient malabsorption.
Nutritional Management
Since celiac disease can lead to nutrient deficiencies due to malabsorption, nutritional management is crucial. Working with a registered dietitian who specializes in celiac disease can help ensure a balanced and nutrient-rich diet. Key nutrients to focus on include:
- Iron: To prevent anemia.
- Calcium and Vitamin D: To support bone health.
- Folate, Vitamin B12, and other B Vitamins: To address deficiencies and promote overall health.
- Fiber: To ensure proper digestion and prevent constipation, especially when many gluten-free products are low in fiber.
A dietitian can recommend gluten-free sources of these nutrients and suggest appropriate supplements if necessary.
Avoiding Cross-Contamination
Cross-contamination with gluten-containing foods is a significant concern for individuals with celiac disease. Here are some strategies to minimize this risk:
- Kitchen Hygiene: Use separate utensils, cutting boards, and appliances for gluten-free and gluten-containing foods. Clean surfaces thoroughly to remove any traces of gluten.
- Dining Out: Communicate clearly with restaurant staff about your dietary needs. Choose restaurants with gluten-free menus or those known for accommodating celiac disease.
- Food Labels: Read labels meticulously to identify hidden sources of gluten. Look for certified gluten-free labels for assurance.
Support Systems
Living with celiac disease can be challenging, but support from family, friends, and community can make a significant difference. Joining a celiac disease support group provides an opportunity to share experiences, recipes, and tips with others who understand the condition. These groups can offer emotional support and practical advice, making the transition to a gluten-free lifestyle smoother.

Monitoring for Associated Conditions
People with celiac disease are at higher risk for other autoimmune conditions, such as thyroid disease and type 1 diabetes. Regular screening for these conditions is important. Additionally, monitoring for conditions like dermatitis herpetiformis, a skin manifestation of celiac disease, ensures comprehensive management of the disease.
Mental Health Considerations
Managing a condition like celiac disease can be stressful and impact mental health. Anxiety, depression, and feelings of isolation are not uncommon. Seeking support from mental health professionals, such as counselors or therapists, can help address these challenges. Mindfulness practices, stress management techniques, and maintaining a strong support network can also contribute to better mental health.
By adopting a holistic approach to managing celiac disease, individuals can drastically improve their quality of life, reduce symptoms, and prevent long-term complications. Consistent medical follow-ups, proper nutritional management, and strong support systems are key components of effective celiac disease management.
Prevalence of Celiac Disease
Celiac disease affects about 1.4% of the global population based on blood tests and about 0.7% based on biopsy results. The prevalence varies by region, with higher rates in Europe and Oceania (0.8%) and lower rates in South America (0.4%), Africa, and North America (0.5%) (Celiac Disease Foundation) (World Population Review). In the United States, the prevalence has remained relatively stable over recent years, affecting approximately 0.7% of the population (JAMA Network).
Accuracy of the tTG Blood Test
The Tissue Transglutaminase (tTG) Blood Test is highly accurate, with a sensitivity and specificity of approximately 98%. This makes it one of the most reliable tests for diagnosing celiac disease.
Impact of a Gluten-Free Diet
Studies show that most individuals with celiac disease experience significant symptom relief within weeks to months of starting a gluten-free diet. The majority of patients also show a decrease in tTG antibody levels, indicating reduced immune activity and intestinal healing.
Long-Term Health Outcomes
Proper management of celiac disease with a gluten-free diet can prevent long-term complications such as osteoporosis, infertility, and increased risk of certain cancers. Getting diagnosed early and adherence to a gluten-free diet are crucial in preventing these complications.
Economic Impact
Maintaining a gluten-free diet can be more expensive because of food gluten-free products can be more exspensive. Additionally, undiagnosed or poorly managed celiac disease can lead to increased healthcare costs from complications and frequent doctor visits (Go Gluten Freely).
For further information, you can refer to the detailed articles and studies available through the Celiac Disease Foundation and other reputable sources such as the JAMA Network and World Population Review.
Conclusion
In summary, the Tissue Transglutaminase (tTG) Blood Test is a critical tool for diagnosing celiac disease. This test detects the presence of tTG IgA antibodies, which are typically elevated in individuals with untreated celiac disease. A positive tTG blood test strongly suggests the presence of celiac disease, which can be confirmed with an intestinal biopsy. It is important to comprehend the implications of the test results and to take necessary actions following a positive diagnosis. This may involve seeking advice from a gastroenterologist and making the switch to a gluten-free diet, which are essential steps in managing the condition.
Celiac disease affects about 1.4% of the global population and has varying prevalence across regions. Accurate diagnosis and effective management can significantly improve symptoms and prevent long-term complications. Adopting a gluten-free diet, seeking regular medical follow-ups, and leveraging support systems are essential components of managing celiac disease.
Ongoing research continues to explore and find new treatments and improve our understanding of this condition. As we learn more, the hope is to provide better support and options for those living with the complications of celiac disease. If you suspect you might have celiac disease or have been diagnosed, consulting with healthcare professionals and taking proactive steps toward management can help you lead a healthy and fulfilling life. The first step is to get tested, and you can do that with a blood test that you can purchase here.